Cracked Heels and How to Prevent Them
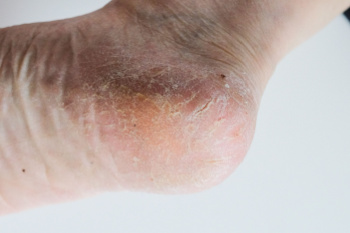
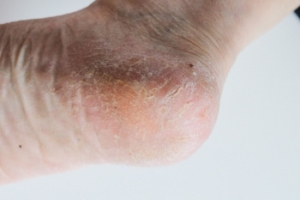
Cracked heels, also known as heel fissures, are characterized by dry, thickened skin on the heels that splits or cracks. This condition often occurs due to factors such as dry weather, excessive standing or walking, improper footwear, or lack of proper foot care. When the skin becomes dry and loses its elasticity, it can crack under pressure, leading to painful fissures that may bleed or become infected, if left untreated. Prevention of cracked heels involves regular moisturizing to keep the skin hydrated and supple. Use a thick, emollient foot cream or lotion containing ingredients like urea or glycerin to help soften and moisturize dry skin. Exfoliating the heels regularly with a pumice stone or foot file can help remove dead skin cells and prevent the buildup of calluses. Additionally, wearing properly fitting shoes with adequate support and cushioning can reduce pressure on the heels and minimize the risk of developing cracked heels. If you have developed cracked heels that persist or become infected, it is strongly suggested that you visit a podiatrist for treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
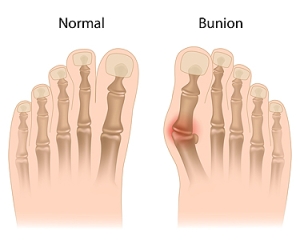
Treatment Options for Bunions
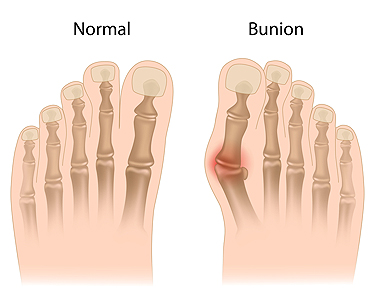
Bunions, medically termed hallux valgus, are a foot deformity characterized by a bony bump at the base of the big toe, while the top of the toe shifts toward the others. Bunions are often accompanied by inflammation and pain. Factors like hereditary predisposition and wearing tight or improper footwear can worsen the deformity. Treatment strategies for bunions typically encompass both non-surgical and surgical approaches. Non-surgical intervention focuses on symptom management and includes wearing well-fitted shoes that provide ample space for the toes. Wearing bunion pads, toe spacers, or orthotic devices for support are among the less invasive treatment options. However, if conservative measures fail to provide relief or if the bunion is severe, surgery may be necessary. Bunion surgery aims to realign the toe joint, alleviate pain, and improve foot function. Surgical techniques include joint trimming and total joint replacement, depending on the severity of the bunion. If you have a bunion that is affecting your daily activities, it's suggested that you schedule an appointment with a podiatrist for a thorough exam and suggested treatment measures.
If you are suffering from bunion pain, contact one of our podiatrists of Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Heel Pain in Tennis Players
 Heel pain is a frequent issue for tennis players. The sport involves intense footwork, with quick lateral movements and repetitive impact. Plantar fasciitis and heel spurs are two of the most common conditions for heel pain in tennis players. Plantar fasciitis occurs when the plantar fascia, a thick band of tissue running along the bottom of the foot, becomes strained and irritated from continuous activity. Heel spurs are bony growths on the heel bone and often develop in response to the chronic strain, pulling, and inflammation of the plantar fascia. Symptoms typically include a sharp, stabbing pain in the bottom of the foot near the heel, especially noticeable during the first steps after waking up or after long periods of rest. To manage and treat these conditions, tennis players may be advised to wear shoes with adequate cushioning and support, engage in proper warm-up and stretching exercises before playing, and incorporate rest days into their training schedules. It is important to get appropriate treatment for these conditions to prevent them from worsening. Podiatrists, or foot doctors, can suggest specialized treatments such as custom orthotics, targeted stretching, or even corticosteroid injections to alleviate pain and prevent further injury. If you are a tennis player with heel pain, it is suggested that you make an appointment with a podiatrist for treatment.
Heel pain is a frequent issue for tennis players. The sport involves intense footwork, with quick lateral movements and repetitive impact. Plantar fasciitis and heel spurs are two of the most common conditions for heel pain in tennis players. Plantar fasciitis occurs when the plantar fascia, a thick band of tissue running along the bottom of the foot, becomes strained and irritated from continuous activity. Heel spurs are bony growths on the heel bone and often develop in response to the chronic strain, pulling, and inflammation of the plantar fascia. Symptoms typically include a sharp, stabbing pain in the bottom of the foot near the heel, especially noticeable during the first steps after waking up or after long periods of rest. To manage and treat these conditions, tennis players may be advised to wear shoes with adequate cushioning and support, engage in proper warm-up and stretching exercises before playing, and incorporate rest days into their training schedules. It is important to get appropriate treatment for these conditions to prevent them from worsening. Podiatrists, or foot doctors, can suggest specialized treatments such as custom orthotics, targeted stretching, or even corticosteroid injections to alleviate pain and prevent further injury. If you are a tennis player with heel pain, it is suggested that you make an appointment with a podiatrist for treatment.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Foot Injuries From Pickleball

Pickleball, a rapidly growing sport appealing to all ages and skill levels, combines elements of tennis, badminton, and ping pong. Played on a smaller court with a solid paddle and a perforated plastic ball, it is enjoyed for its simplicity and social aspect. However, like many physical activities, pickleball can pose risks to foot health. Injuries to the feet during pickleball commonly result from strain or overuse due to sudden movements, pivoting, and repetitive footwork. Such injuries may include sprains, strains, and stress fractures. To prevent foot injuries while playing pickleball, it is important to stay active, stretch before and after playing, and engage in other physical activities to maintain overall fitness and foot strength. Additionally, staying hydrated by drinking water helps to prevent muscle cramps and fatigue. If you have persistent foot pain or injuries from playing pickleball, it is suggested that you see a podiatrist. A foot doctor can offer guidance on injury prevention techniques and provide treatment to alleviate discomfort and promote foot health.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact one of our podiatrists of Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
Key Facts About Children’s Athlete’s Foot

Athlete's foot, a fungal infection affecting the skin of the feet, is not exclusive to adults, as children can also fall prey to this uncomfortable condition. Commonly caused by the same fungi responsible for ringworm and jock itch, athlete's foot thrives in warm, moist environments, making children's sweaty feet particularly susceptible. Symptoms can include itching, burning, and redness, often between the toes or on the soles of the feet. Children can contract athlete's foot by walking barefoot in public areas, such as swimming pools, locker rooms, or communal showers. Sharing towels, socks, or shoes with an infected individual can also facilitate transmission. Teaching children proper foot hygiene, such as keeping feet clean and dry, wearing breathable footwear, and avoiding walking barefoot in public spaces, can help prevent athlete's foot and promote overall foot health. If your child has itchy feet, it is suggested that you consult a podiatrist who can properly diagnose and treat athlete’s foot, which may include prescribed medication.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with one of our podiatrists from Summit Podiatry. Our doctors will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.