What Is a Podiatrist, and What Do They Treat?
Podiatrists are physicians that specialize in the foot and ankle. Podiatrists contain the DPM suffix after their name which means they achieved a Doctorate of Podiatric Medicine in medical school. They typically continue their post graduate training with a residency in a clinic or hospital. After passing certain exams, a podiatrist can become board certified by The American Board of Podiatric Medicine. While they treat general foot conditions such as ingrown toenails, heel pain, corns, calluses, bunions, fungal nail infections and more, some podiatrists also specialize in areas such as wound care, diabetes, sports medicine, arthritis, neuromas, gait analysis and correction, custom orthotics, and bunion removal. Certain podiatrists will even specialize in podiatric surgery and, after passing additional exams, may become certified by the American Board of Foot and Ankle Surgery. If you experience any swelling, severe pain, numbness or tingling, or have an open sore on your feet, it is suggested that you call a podiatrist to seek proper treatment.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact one of our podiatrists from Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
Do I Have Morton's Neuroma?
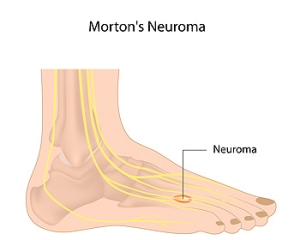
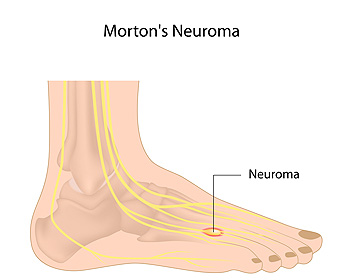 Morton’s neuroma is a painful foot condition caused by damage to the nerve between the third and fourth toes. The tissue that surrounds the nerve thickens due to inflammation, causing symptoms such as toe numbness, a tingling sensation, a feeling akin to “walking on a pebble,” and burning pain in the ball of the foot. Morton’s neuroma is eight to ten times more common in women than in men because it is believed to be caused by wearing ill-fitting shoes. Morton's neuroma can also result from damaging the foot during high impact sports or from other trauma to the nerves of the feet. Having certain foot deformities, such as flat feet, high arches, hammertoes, or bunions, can also put you at an increased risk of developing Morton’s neuroma. If you have symptoms of this condition, please seek the care of a podiatrist.
Morton’s neuroma is a painful foot condition caused by damage to the nerve between the third and fourth toes. The tissue that surrounds the nerve thickens due to inflammation, causing symptoms such as toe numbness, a tingling sensation, a feeling akin to “walking on a pebble,” and burning pain in the ball of the foot. Morton’s neuroma is eight to ten times more common in women than in men because it is believed to be caused by wearing ill-fitting shoes. Morton's neuroma can also result from damaging the foot during high impact sports or from other trauma to the nerves of the feet. Having certain foot deformities, such as flat feet, high arches, hammertoes, or bunions, can also put you at an increased risk of developing Morton’s neuroma. If you have symptoms of this condition, please seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Summit Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Why Foot Wounds Are Problematic for Diabetics
Millions of people in America suffer from diabetes, which often leads to complications in their feet. Diabetes impairs the body’s ability to regulate blood glucose levels. This, in turn, disrupts the functionality of white blood cells which are critical in closing wounds. Additionally, diabetes can lead to poor circulation, and this reduces the amount of nutrients sent to wound sites and further impairs the healing process. Neuropathy, or nerve damage, is another condition associated with diabetes. Neuropathy further complicates diabetic wound management because it can prevent diabetic adults from feeling when there is trauma or an injury to their skin, and wounds may progress before they are even discovered. All of these factors combined make the diabetic wound harder to detect and heal, which may lead to infection and worse—if it's not treated properly. If you are diabetic, it's important to be under the care of a podiatrist who can offer preventative measures against foot wounds and treat them promptly and properly if they do develop.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Summit Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Why Live with Pain and Numbness in Your Feet?
The Types of Hammertoes
 Hammertoe occurs when the ligaments and tendons in the middle joint of toes tighten up and force the toes to curl downwards. This can normally happen in any toe except the big toe. The hammertoe can often become uncomfortable if it rubs against the shoe. There are two types od hammertoes which are categorized by the affected toe’s mobility. Flexible hammertoes can be straightened out manually. However, a rigid hammertoe can not be manually straightened out, and its movement can be very limited and painful. Those who are suffering from hammertoes should make sure to wear shoes with a high and wide toe box that allows for enough space for the toes. If your hammertoes persist, make sure to consult with a podiatrist for treatment options since surgery may be necessary.
Hammertoe occurs when the ligaments and tendons in the middle joint of toes tighten up and force the toes to curl downwards. This can normally happen in any toe except the big toe. The hammertoe can often become uncomfortable if it rubs against the shoe. There are two types od hammertoes which are categorized by the affected toe’s mobility. Flexible hammertoes can be straightened out manually. However, a rigid hammertoe can not be manually straightened out, and its movement can be very limited and painful. Those who are suffering from hammertoes should make sure to wear shoes with a high and wide toe box that allows for enough space for the toes. If your hammertoes persist, make sure to consult with a podiatrist for treatment options since surgery may be necessary.
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists of Summit Podiatry. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Types of Heel Pain
 Research has indicated that there are several forms of heel pain. The most common type is referred to as plantar fasciitis, and this occurs as a result of an inflamed plantar fascia. This is the band of tissue that is located on the sole of the foot, connecting the heel to the toes. Heel bursitis is a condition where pain is felt in the middle of the heel, and can develop as a result of falling from an extended height. Young children who participate in sporting activities may develop Sever’s disease, and this may develop from an inflamed Achilles tendon. Many patients will experience heel pain at some point in their lives, and there are methods to managing the pain and discomfort. If you have any type of heel pain, it is advised to consult with a podiatrist who will perform a proper diagnosis, and begin the correct treatment.
Research has indicated that there are several forms of heel pain. The most common type is referred to as plantar fasciitis, and this occurs as a result of an inflamed plantar fascia. This is the band of tissue that is located on the sole of the foot, connecting the heel to the toes. Heel bursitis is a condition where pain is felt in the middle of the heel, and can develop as a result of falling from an extended height. Young children who participate in sporting activities may develop Sever’s disease, and this may develop from an inflamed Achilles tendon. Many patients will experience heel pain at some point in their lives, and there are methods to managing the pain and discomfort. If you have any type of heel pain, it is advised to consult with a podiatrist who will perform a proper diagnosis, and begin the correct treatment.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Summit Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.