What to Do With a Broken Toe

A broken toe can cause sudden pain, swelling, bruising, and difficulty walking. The toe may appear crooked or misaligned, and in some cases, you might hear a popping sound at the time of injury. Common causes of broken toes include dropping heavy objects on the foot, stubbing your toe, or sports-related accidents. Treatment for a broken toe often involves elevation to reduce swelling and pain. Depending on the severity of the fracture, your podiatrist may recommend buddy taping the toe or using a special shoe to protect it while it heals. In more severe cases, surgery may be needed to realign the bones. While many broken toes can heal on their own, it is important to visit a podiatrist to ensure the injury is properly diagnosed and treated. Improper treatment can lead to long-term pain or deformity. If you think you may have a broken toe, it is suggested that you make an appointment with a podiatrist.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact one of our podiatrists from Summit Podiatry. Our doctors will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
What is Capsulitis of the Foot?

Capsulitis of the foot is an inflammation of the ligament-like capsule surrounding a joint, most commonly affecting the second toe at the ball of the foot. It occurs when excessive pressure or stress causes irritation, often due to improper footwear, abnormal foot mechanics, or activities that involve repetitive forefoot impact. People with high arches, flat feet, or a second toe longer than the big toe are more prone to developing capsulitis. Symptoms include pain under the ball of the foot, swelling, and a sensation of walking on a marble. The second toe may also appear elevated or shift out of alignment. Early treatment is important and includes wearing supportive footwear and avoiding high-impact activities. Surgery is rarely needed to correct the issue. If you have symptoms of capsulitis, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Summit Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Facts About Heel Spur Surgery
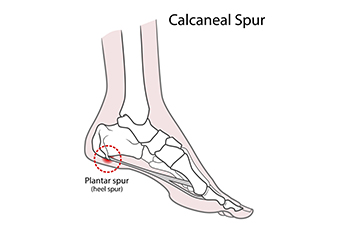
Heel spur surgery may be recommended when chronic heel pain does not improve with non-surgical treatments. Heel spurs are bony outgrowths on the calcaneus, often linked to conditions like plantar fasciitis or Achilles tendonitis. Heel spur surgery aims to alleviate pain by removing the bone spur and addressing the underlying issue. Procedures vary based on the spur's location. Inferior spurs, which develop on the bottom of the heel, are often treated alongside plantar fasciitis release surgery. Posterior spurs, which occur near the Achilles tendon, require more complex techniques. Treatment may involve open surgery or less invasive endoscopic methods, with recovery typically taking several weeks to months. Risks include nerve damage, foot instability, or prolonged discomfort. A podiatrist can guide you through diagnosis, recommend the appropriate treatment, and support your recovery. If you are suffering from heel pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Summit Podiatry. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Are You Suffering From Ingrown Toenails?
Preventing Limb Loss in Diabetics

Preventing lower-limb amputations in people with diabetes involves diligent care and monitoring, especially for foot health. High blood sugar over time can lead to peripheral arterial disease, which reduces blood flow to the feet and makes it more difficult for wounds to heal. Additionally, nerve damage resulting from high blood sugar levels can reduce sensation, leading patients to miss injuries that can worsen and become ulcerated. Even a minor cut can develop into a severe infection if unnoticed or untreated. Regular foot exams by a podiatrist can help identify early signs of complications, such as sores, ulcers, or infections. Through specialized wound care and appropriate treatments, podiatrists play an essential role in helping to prevent problems that could lead to gangrene or ultimately amputation. Promptly addressing any concerns with a podiatrist can significantly reduce the risk of these serious complications. If you have problematic foot ulcers resulting from diabetes, it is suggested that you make regular appointments with a podiatrist.
Limb salvage can be an effective way in preventing the need for limb amputation. If you have diabetes, cancer, or any other condition that could lead to foot amputation if left unchecked, consult with one of our podiatrists from Summit Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Limb Salvage?
Limb salvage is the attempt of saving a limb, such as the foot from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Diabetes is the number one cause of non-traumatic amputations in the United States. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
However, there are other causes as well, such as cancer and traumatic injury. Links between higher mortality rates and amputation have been found. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes, peripheral vascular disease, neuropathy, cancer, and severe crush injury. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If the bone is removed, it is then replaced with prostheses, synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
Comparing Sesamoiditis and Gout

Gout and sesamoiditis are two distinct conditions that affect the big toe and can cause significant foot pain, but their causes, symptoms, and treatments vary greatly. Gout is an inflammatory arthritis triggered by uric acid crystals, frequently forming in the big toe joint. This can cause sudden, intense pain, warmth, and swelling. This painful condition is associated with risk factors like genetics, certain health issues, and a purine-rich diet. Treatment for gout includes medications to manage pain and prevent future attacks. In contrast, sesamoiditis is the inflammation of the tiny sesamoid bones and surrounding tendons at the base of the big toe. It typically occurs from overuse, especially activities that place stress on the ball of the foot, such as running or dancing. Sesamoiditis causes a dull ache that worsens with walking or bearing weight. A podiatrist can determine whether you have gout or sesamoiditis, and offer treatment options for either condition. If your big toe is in pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Summit Podiatry. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Wilmington, Whiteville, and Wallace, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.